Depression and suicide are extremely common among older adults. In the U.S., about 11% of our seniors are diagnosed with some form of depression. This number does not include those who are suffering silently. Some experts believe that the true prevalence of depression among seniors is closer to 30-50%.
As many people age, personal losses on multiple fronts can accumulate – loss of health, loss of ability, loss of work, loss of friends and family…leading to a sense of hopelessness and despair.
The signs of depression can be subtle but if family and friends are able to recognize signs of early depression in an elderly loved one, a senior’s life could be dramatically changed and in some instances, even saved, by a few simple interventions.
Signs and Symptoms of Depression in the Elderly
Loss of interest in usual activities or prior interests and hobbies
- Withdrawal from friends and social interactions
- Disturbances in sleep (difficulty falling asleep or staying asleep, oversleeping, or daytime sleepiness)
- Change in appetite (either increased or decreased)
- Fatigue
- Slowed movement or speech
- Memory problems
- Neglect of personal appearance
- Neglect of the home
- Sense of worthlessness
- Statements of hopelessness, despair and of giving up
- Frequent sighing
Seniors who have chronic illness, who were recently discharged from a hospital stay or are in a nursing home, are at particularly high risk for depression.
When depression is suspected, a doctor should be consulted. Firstly, many sufferers could benefit from anti-depressant medications. Secondly, medical conditions such as low thyroid hormone, early Parkinson’s disease or Alzheimer’s dementia can present as depression and should be treated as well. Depression is encountered more frequently among seniors who have heart disease, diabetes, history of stroke and cancer, compared to the general population. Thirdly, your primary care doctor can refer you to a specialist such as a psychiatrist and/or psychologist.
Many medications can cause or worsen depression including:
- Blood pressure medication (clonidine)
- Beta-blockers (e.g. Lopressor, Inderal)
- Heart drugs containing reserpine
- Calcium-channel blockers
- High-cholesterol drugs (e.g. Lipitor, Mevacor, Zocor)
- Painkillers and arthritis drugs
- Ulcer medication (e.g. Zantac, Tagamet)
- Steroids (e.g. cortisone and prednisone)
- Estrogens (e.g. Premarin, Prempro)
- Sleeping pills
- Tranquilizers (e.g. Valium, Xanax, Halcion)
- Medications for Parkinson’s disease
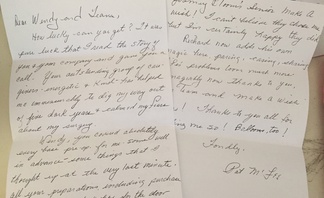
it can be difficult to maintain perspective and sustain the effort required to beat depression. That’s why support from family and friends matter. A simple phone call can be the highlight of someone’s day however digital communication isn’t a replacement for face-to-face contact. It’s still best to see people in person on a daily basis.
Family and friends can mitigate depression by providing support in many ways:
- Simply spending time together
- Listening in a supportive and non-judgmental manner
- Going out on outings
- Encouraging learning new skills
- Building new friendships
- Thoughtful small gifts and other tokens of affection
- Creating opportunities to laugh – whether it’s jokes, comedy movies, funny books or an improve show.
- Talking openly about depression - It is a misconception that family and friends should avoid talking about depression. In severe depression, it’s even acceptable to ask if a suicide plan has been made.
- Encouraging healthy lifestyle habits (see next section)
When depressed, it’s hard to find the motivation to do anything—let alone maintain healthy lifestyle habits. Family and friends can be instrumental in promoting healthy habits. When the body is taken care of, it’s easier to achieve mental well-being.
Here are some healthy lifestyle habits:
- Exercise - is a powerful depression treatment. In fact, research suggests it can be just as effective as antidepressants. A little physical activity can do wonders. Anything that involves getting up and moving helps. Look for small ways to add more movement to the day: parking farther from the store, taking the stairs,
- Dietary habits make a difference with depression. Start by minimizing sugar and refined carbs. Sugary and starchy comfort foods can give the body a quick boost, but later on when the blood sugar crashes, depression can be worsened. Instead, focus on quality protein, complex carbs, and healthy fats, which leave the body feeling satisfied and do not cause emotional swings. Going too long without eating can also worsen mood swings and feelings of tiredness and irritability. In addition to the three meals a day, we encourage small healthy snacks in between so that there is food intake at least every 3-4 hours.
- Good sleep habits are very important. Many older adults struggle with sleep problems, particularly insomnia. But lack of sleep makes depression worse. Aim for somewhere between 7 to 9 hours of sleep each night. Good sleep habits include: avoiding alcohol and caffeine, keeping a regular sleep-wake schedule, and making sure the bedroom is dark, quiet, and cool.
Depression is not a normal or necessary part of aging. Senior depression can be treated, and with the right support, treatment, and self-help strategies, yourself or a loved one suffering from depression can live a vibrant and happy life!